Bariatric Weight-loss Surgery
Bariatric surgery can help contribute to an individual’s weight loss by restricting the amount of food the stomach can hold and reduction in calorie absorption in the stomach and small intestines.
Weight loss surgery can cure or improve diabetes, sleep apnea, hypertension, and many other obesity related diseases. Weight loss surgery followed by significant weight-loss can lead to significant benefits including decreased chance of heart attack or stroke. Each bariatric weight loss surgery has its own advantages and disadvantages. Sometimes the most effective long-term management for obesity is bariatric surgery. Bariatric procedures can often cause hormonal changes.
Bariatric weight loss surgery is achieved by reducing the size of the stomach with a gastric band, or through removal of a portion of the stomach, or by re-routing the small intestine to a small stomach pouch (gastric bypass surgery). Most weight loss surgeries are performed via laparoscopic surgery because it is the least invasive technique.
The most common bariatric surgery procedures are gastric bypass, sleeve gastrectomy, adjustable gastric band, and biliopancreatic diversion with duodenal switch.
Who Qualifies For Weight-loss Surgery
The National Institute of Health (NIH) recommends bariatric surgery for obese people with a body mass index (BMI) of at least 40.
If diet, exercise, and other weight-loss methods haven’t worked, bariatric surgery may be the right choice to better your health and gain an improved quality of life. Our bariatric surgery program addresses the physical, mental and emotional challenges of weight-loss surgery by developing a specifically designed personalized care plan.
Some other health benefits from weight-loss can include:
Increase in HDL (good) cholesterol
Lowering in both systolic and diastolic blood pressure
Decreased risk of diabetes
Improvement in cardiovascular factors
Reduction in mortality
Minimally-invasive Bariatric Weight-loss Procedures:
Bariatric weight-loss surgery includes several different procedures performed on people who have obesity.
Gastric Bypass Surgery – The surgeon creates a small stomach pouch that restricts the amount of food you can eat. The digestive tract is rerouted, which helps decrease the amount of nutrients, fat and calories your body absorbs.
Vertical Sleeve Gastrectomy – The stomach is reduced to about 1/5 of its original size by removing a large portion of the stomach resulting in a sleeve or tube like structure. This procedure is not reversible.
Gastric Band Surgery (Lap Band) – A silicone band with an inflatable ring is placed around the stomach to slow the passage of food from the upper stomach to the lower stomach area. The Lap Band allows for the adjustment of the band to meet the patient’s needs and desires.
Biliopancreatic Diversion with Duodenal Switch (BPD/DS) Gastric Bypass – This procedure creates a new, smaller stomach by removing most of the main stomach. Then a large portion of the small intestine is bypassed. The BPD/DS is considered to be the most effective bariatric surgery for the treatment of diabetes.
Endoscopic Gastric Balloon (Non-surgical procedure) – A single or dual balloon is inserted through an endoscope into the stomach. The balloon is then filled with a saline solution, which will help the patient feel fuller faster when they eat. This minimally-invasive balloon system option is designed to stay in place for six months or less.
Revisional surgeries and procedures– Our bariatric surgeons can review any previous weight-loss surgery that did not achieve their desired outcomes for whatever reason. Other revisional procedures can include lap band removal and other conversion gastrectromy procedures.
Gastric Bypass Surgery
The Gastric Bypass is considered the ‘gold standard’ of weight loss surgery. There are two components to the procedure.
First, a small stomach pouch is created by dividing the top of the stomach from the rest of the stomach.
Then the first portion of the small intestine is divided, and the bottom end of the divided small intestine is brought up and connected to the newly created small stomach pouch.
The top portion of the divided small intestine is then connected to the small intestine further down so that the stomach acids and digestive enzymes from the bypassed stomach and first portion of small intestine will eventually mix with the food.
This newly created stomach pouch is much smaller and facilitates significantly smaller meals, which equals fewer calories consumed. Additionally, because there is less digestion of food with the new smaller stomach, the segment of small intestine that would normally absorb calories now no longer has food going through it.
This rerouting of the food stream can produce healthy changes such as weight-loss, suppress hunger, and maybe help reduce type 2 diabetes associated with obesity. The Gastric Bypass procedure also helps restrict the amount of food that can be consumed which produces significant long-term weight loss.
Some of the disadvantages of the Gastric Bypass procedure include a longer hospital stay after the procedure. It is also important that the patient continues to follow dietary recommendations, life-long vitamin / mineral supplementation, and follow-up visits to make sure the patient is healthy for the rest of their life.
Vertical Sleeve Gastrectomy
The Laparoscopic Sleeve Gastrectomy is performed by removing almost 80 percent of the stomach. The remaining small section of the stomach is a pouch that resembles a banana.
The newly created small stomach pouch obviously can only hold considerably smaller volumes which will help significantly in reducing the amount of food / calories that can be consumed.
As with any procedure that modifies the stomach or digestive area, this surgery can have a greater effect on gut hormones produced by the stomach that impact a number of factors including hunger, satiety, and blood sugar control.
Even though this procedure has advantages including restricting the amount of food the stomach can hold, however, this procedure is non-reversible, has a higher potential for long-term vitamin deficiencies, and even has a higher early complication rate than the Gastric Bypass procedure.
Adjustable Gastric Band Surgery (Lap Band)
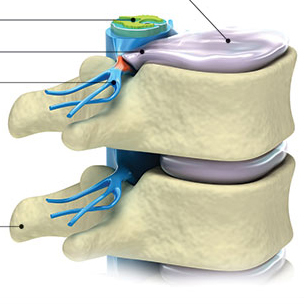
The Adjustable Gastric Band – often called the band – involves an inflatable band that is placed around the upper portion of the stomach, creating a small stomach pouch above the band, and the rest of the stomach below the band.
This device works by creating a smaller stomach pouch, so eating just a small amount of food will satisfy hunger and promote feeling full. How ‘full’ the stomach feels depends upon the size of the opening between the pouch and the remainder of the stomach created by the gastric band. The band helps in that it reduces hunger, which helps patients decrease the amount of calories that are consumed during a day.
The size of the stomach opening is adjustable by filling the band with sterile saline, which is injected through a port placed under the skin. Reducing the size of the opening is done gradually over time with repeated adjustments.
What is an important difference about this device is that there is no malabsorption, so any food that is consumed will be digested and absorbed, as the stomach would normally operate.
Some of the advantages of this procedure include reduction in food intake, loss of weight, less than 24 hour hospital stay, discharged same day, and involves no cutting of the stomach or rerouting of the intestines, so the procedure is reversible and adjustable if necessary. This procedure also has the lowest rate of postoperative complications and also has the lowest risk for vitamin / mineral deficiencies.
Some of the disadvantages may include slower weight loss than other surgical options, a foreign device remains in the body, or mechanical problems with the band or filling area that have to be surgically fixed.
Biliopancreatic Diversion with Duodenal Switch (BPD/DS) Gastric Bypass
The Biliopancreatic Diversion with Duodenal Switch is a procedure that first creates a new smaller, stomach pouch by removing part of the stomach. Then a large portion of the small intestine is bypassed. The BPD/DS is considered to be the most effective bariatric surgery for the treatment of diabetes.
The first portion of the small intestine is called the duodenum, which helps assist with digestion and absorbing nutrition. A segment of the small intestine is brought up and connected to the outlet of the newly created stomach, bypassing roughly 75% of the small intestine. So that when the patient eats, food travels through the newly created stomach pouch and enters directly into the last part of the small intestine.
The bypassed small intestine is reconnected to the last portion of the small intestine in order to allow stomach / digestive enzymes able to mix with the food stream.
With this reconnection at the lower end of the food stream, the food intake will not mix with the normal digestive enzymes until the food gets very far down the small intestines creating a significant decrease in the absorption of calories and nutrients.
One of the bigger advantages of this bariactric surgery is that it is most effective against diabetes and also reduces the absorption of fat by over 50%, contributing to extra weight loss.
However, this surgery requires a longer hospital stay, plus there is a higher chance of continuous nutrition deficiency if adequate food treatment plans are not followed. Mismanagement of continuous food intake can lead to protein deficiencies and long-term deficiencies in vitamins and minerals.